Medical insurance serves as the cornerstone of healthcare financing, ensuring access to essential services while managing financial risks for patients and providers. The revenue cycle, a critical process in healthcare administration, encompasses all activities from patient registration to payment collection, ensuring seamless financial operations. Understanding this cycle is vital for optimizing healthcare delivery and maintaining sustainable business practices.
1;1 Overview of Medical Insurance
Medical insurance is a financial arrangement that protects individuals and families from healthcare costs, ensuring access to essential medical services. It involves agreements between patients, providers, and payers to share the financial burden of healthcare. Various types of plans, such as HMOs, PPOs, and CDHPs, offer different levels of coverage and flexibility. Accurate billing and coding are critical for seamless claims processing. The revenue cycle process, as detailed in “Medical Insurance: A Revenue Cycle Process Approach,” emphasizes ten steps to manage claims effectively, ensuring providers receive timely reimbursement while maintaining patient care quality.
1.2 Importance of the Revenue Cycle in Healthcare
The revenue cycle is integral to healthcare operations, ensuring financial sustainability and efficient patient care delivery. It streamlines processes from registration to reimbursement, minimizing delays and errors. An optimized cycle enhances provider profitability, reduces operational costs, and improves patient satisfaction. Effective revenue cycle management (RCM) ensures accurate claims submission, minimizes denials, and accelerates payments, enabling healthcare organizations to focus on quality care. A well-managed cycle also supports compliance with regulatory requirements, maintaining trust and transparency between patients, providers, and payers. Its importance extends to the overall stability and growth of the healthcare system.
Key Components of the Revenue Cycle Management (RCM) Process
The RCM process includes patient registration, eligibility verification, charge capture, coding, claims submission, processing, reimbursement, and payment posting. These steps ensure seamless financial transactions and compliance.
2.1 Patient Registration and Eligibility Verification
Patient registration and eligibility verification are the initial steps in the RCM process. Accurate patient data collection ensures proper identification and billing. Eligibility verification confirms insurance coverage, reducing billing errors and denied claims. Automated tools streamline this process, improving efficiency and accuracy. Verifying benefits before service delivery ensures providers understand coverage limits and patient responsibilities. This step is critical for avoiding financial discrepancies and ensuring smooth claims processing. Effective communication with patients about their financial responsibilities enhances transparency and satisfaction. Proper registration and verification lay the foundation for a seamless revenue cycle, minimizing delays and errors in subsequent steps.
2.2 Charge Capture and Coding
Charge capture and coding are essential steps in the revenue cycle, ensuring accurate billing and reimbursement. Charge capture involves documenting all services provided, while coding translates these services into standardized codes (e.g., ICD-10-CM, CPT). Accurate coding ensures compliance with regulations and proper reimbursement. Errors in coding can lead to claim denials or revenue loss. Efficient charge capture and coding processes are critical for maintaining financial integrity and ensuring providers receive timely payment for services rendered. This step bridges patient care and billing, making it a cornerstone of effective revenue cycle management.
2.3 Claims Submission and Processing
Claims submission and processing involve sending accurately coded bills to insurance companies for reimbursement. This step ensures that healthcare providers receive payment for services rendered. Claims can be submitted electronically or via paper, with electronic submission being faster and less error-prone. Insurance companies review claims for accuracy, eligibility, and adherence to policies. Approved claims are reimbursed, while denied claims require follow-up to resolve issues. Efficient claims processing is crucial for maintaining cash flow and reducing revenue cycle delays. Accurate data entry and adherence to payer guidelines are essential to minimize denials and ensure timely payments. This step is vital for healthcare financial sustainability.
2.4 Reimbursement and Payment Posting
Reimbursement and payment posting mark the final stages of the revenue cycle, where healthcare providers receive payment for services rendered. Insurance companies issue payments based on approved claims, and these funds are posted to the appropriate patient accounts. Accurate posting ensures financial records are up-to-date and reflects the correct balance. Reimbursement rates vary by payer and policy, with payments often adjusted for deductibles, copays, or contractual agreements. Proper management of this step is critical for maintaining financial stability and ensuring seamless patient account resolution. It also fosters trust and transparency between providers, payers, and patients.
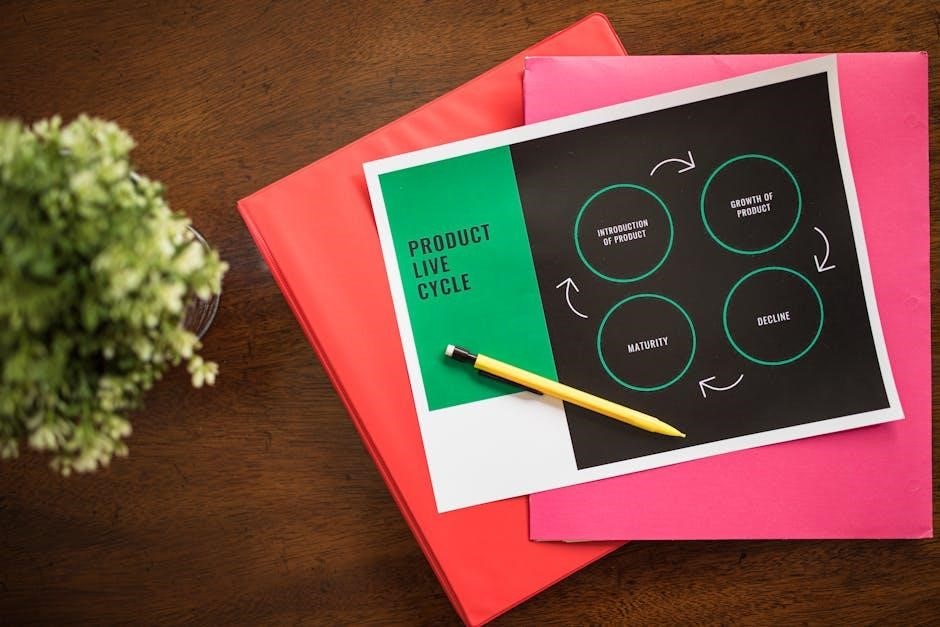
The 10-Step Revenue Cycle Process
The 10-step revenue cycle process streamlines healthcare financial operations, ensuring efficiency and accuracy. It outlines key activities from patient registration to final payment, optimizing revenue management.
The 10-Step Revenue Cycle Model provides a structured framework for managing healthcare finances effectively. It outlines the sequential process from patient registration to final payment collection, ensuring transparency and efficiency. This model is essential for healthcare professionals to understand, as it breaks down complex financial operations into manageable steps. By following these steps, organizations can optimize revenue generation, reduce claim denials, and maintain compliance with regulatory requirements. The model emphasizes a patient-centric approach, ensuring accurate billing and timely reimbursements. Its clear structure makes it a valuable tool for streamlining the revenue cycle and improving overall financial performance in healthcare settings.
3.2 Step 1: Patient Registration and Data Collection
Step 1 of the 10-Step Revenue Cycle Model focuses on patient registration and data collection. This initial phase involves gathering accurate patient information, including demographic details, insurance coverage, and financial responsibilities. Proper data collection ensures eligibility verification and smooth processing of claims. Accurate registration is critical, as errors at this stage can lead to delays or denials in reimbursement. Efficient data collection also supports compliance with regulatory requirements and streamlines subsequent steps in the revenue cycle. This step sets the foundation for effective revenue cycle management, emphasizing the importance of precise and comprehensive patient data entry. Its impact is felt throughout the entire process.
3.3 Step 2: Insurance Verification and Eligibility
Step 2 involves verifying a patient’s insurance coverage and eligibility to ensure accurate billing and reimbursement. This step confirms the details of the patient’s policy, including active coverage, deductibles, copays, and any restrictions. Eligibility verification prevents claim denials by ensuring services are covered under the patient’s plan. Automated systems streamline this process, reducing errors and delays. Accurate verification also informs patients of their financial responsibilities, fostering transparency and trust. This step is crucial for maintaining a smooth revenue cycle and minimizing administrative burdens for healthcare providers; Proper verification ensures compliance with payer guidelines and avoids costly rework. It is a foundational element of effective revenue cycle management.
3.4 Step 3: Service Delivery and Charge Capture
Step 3 focuses on delivering medical services and accurately capturing charges for billing purposes. During service delivery, healthcare providers document treatments, procedures, and supplies used. Charge capture ensures that all services rendered are recorded and translated into billable charges. This involves assigning appropriate codes for diagnoses and procedures, ensuring compliance with coding guidelines. Accurate charge capture is essential for preventing revenue loss and ensuring timely reimbursement. It relies on clear communication between clinical staff and billing specialists to maintain data integrity. Effective charge capture systems streamline the billing process, reducing errors and enhancing overall revenue cycle efficiency. This step is vital for maintaining financial accuracy and operational efficiency.
Technological Advancements in Revenue Cycle Management
AI and automation are revolutionizing RCM, enhancing efficiency, accuracy, and sustainability. These technologies optimize workflows, reduce errors, and streamline processes, ensuring better financial outcomes for healthcare providers.
4.1 Role of Artificial Intelligence (AI) in RCM
Artificial Intelligence (AI) significantly enhances Revenue Cycle Management (RCM) by automating complex processes, improving accuracy, and reducing operational inefficiencies. AI-driven tools optimize eligibility verification, claim processing, and payment posting, minimizing manual errors. Predictive analytics powered by AI identifies potential issues before they escalate, such as claim denials, enabling proactive resolutions. Additionally, AI improves patient communication by generating personalized explanations of benefits and payment plans. By streamlining workflows and reducing administrative burdens, AI ensures faster reimbursement cycles and better financial outcomes for healthcare providers. Its integration into RCM is essential for modernizing and sustaining efficient healthcare financial systems.
4.2 Automation and Its Impact on Revenue Cycle Efficiency
Automation revolutionizes the revenue cycle by streamlining processes, reducing manual tasks, and enhancing accuracy. Automated systems efficiently handle eligibility verification, claim submission, and payment processing, minimizing delays and errors. Advanced tools optimize coding, reduce claim denials, and improve reimbursement rates. Automation also enables real-time monitoring and analytics, allowing healthcare providers to identify bottlenecks and improve operational efficiency. By reducing administrative burdens, automation fosters faster revenue cycles, enhances patient satisfaction, and strengthens financial performance. Its integration is critical for modern healthcare organizations aiming to achieve sustainable and efficient revenue cycle management.
Optimizing the Revenue Cycle for Maximum Efficiency
Optimizing the revenue cycle involves streamlining processes, enhancing accuracy, and reducing claim denials. Implementing advanced technologies and best practices ensures efficient financial operations and improved patient satisfaction.
5.1 Best Practices for Reducing Claim Denials
Reducing claim denials requires proactive measures such as thorough patient eligibility verification, accurate coding, and detailed documentation. Regular audits and staff training ensure compliance with payer policies, minimizing errors. Implementing automated claim scrubbing tools helps identify issues before submission, improving first-pass acceptance rates. Clear communication with both patients and payers fosters transparency, resolving issues promptly. By adopting these best practices, healthcare providers can significantly lower denial rates, streamline revenue cycles, and enhance overall financial performance.
5.2 Streamlining the Billing and Coding Process
Streamlining the billing and coding process involves implementing advanced technologies and standardized protocols to enhance accuracy and efficiency. Utilizing AI-driven tools can automate coding, reducing manual errors and ensuring compliance with regulations. Accurate and up-to-date coding structures, such as ICD-10-CM and CPT, are essential for minimizing claim denials. Additionally, regular training for staff on payer-specific rules and documentation requirements can significantly reduce errors. By integrating these strategies, healthcare organizations can achieve faster reimbursement cycles and improve overall revenue cycle performance while maintaining compliance with evolving regulatory standards.
5.3 Strategies to Minimize Revenue Leakage
Minimizing revenue leakage requires a proactive approach to identifying and addressing gaps in the revenue cycle. Implementing robust claim scrubbing tools and conducting regular audits can help detect and correct errors before claims are submitted. Enhancing patient communication to ensure accurate insurance information and upfront collections can also reduce denied claims. Additionally, leveraging technology to track key performance indicators (KPIs) and monitor trends in revenue cycle performance allows organizations to pinpoint and resolve issues promptly. By adopting these strategies, healthcare providers can prevent financial losses and maintain a stable revenue flow.

The Role of Medical Billing and Coding in the Revenue Cycle
Medical billing and coding are essential for translating patient services into claims, using standardized codes like ICD and CPT to ensure accurate reimbursement and compliance with regulations.
6.1 Understanding Medical Billing and Coding Processes
Medical billing and coding are critical processes that convert healthcare services into structured data for insurance claims. Billing involves preparing invoices for services rendered, while coding assigns standardized codes (e.g., ICD-10, CPT) to diagnoses and procedures. These codes ensure accurate communication between providers and payers, facilitating reimbursement. Accurate coding is essential for compliance with regulations and preventing claim denials. The process begins with patient registration, followed by charge capture, coding, and claim submission. Efficient billing and coding ensure timely payments and maintain financial stability for healthcare organizations. Proper training and updates are vital to stay current with coding guidelines and payer policies.
6.2 Impact of Coding Structures on Revenue Cycle Accuracy
Coding structures play a pivotal role in ensuring accuracy throughout the revenue cycle. Accurate and compliant coding directly impacts claim processing, reimbursement, and overall financial performance. Standardized codes, such as ICD-10 and CPT, facilitate clear communication between healthcare providers and payers, reducing errors and denials. Proper coding ensures adherence to regulatory requirements, minimizing legal risks and audits. Incorrect or incomplete codes can lead to delayed payments, revenue leakage, or even fraud investigations. Therefore, precise coding is essential for maintaining integrity and efficiency in the revenue cycle, ensuring that healthcare organizations receive fair compensation for services rendered.

Regulatory and Compliance Considerations
Regulatory compliance is crucial for ensuring accurate claims processing and avoiding legal risks. Adhering to payer policies and coding guidelines minimizes errors and enhances revenue cycle accuracy.
7.1 Understanding Payer Policies and Guidelines
Understanding payer policies and guidelines is essential for effective revenue cycle management. Each payer has specific rules regarding claim submissions, billing codes, and documentation requirements. Adhering to these guidelines ensures timely reimbursements and reduces denial rates. Payer policies often include details on covered services, pre-authorization requirements, and payment terms. Staying updated on these policies is crucial, as they frequently change. By aligning practices with payer expectations, healthcare providers can optimize their revenue cycle, minimize compliance risks, and improve overall financial performance.
7.2 Navigating Regulatory Changes in the Revenue Cycle
Regulatory changes in healthcare significantly impact the revenue cycle, requiring continuous adaptation to maintain compliance. Updates to coding systems, such as ICD-10, and evolving privacy laws like HIPAA, demand precise implementation. Payers often adjust reimbursement policies, affecting how claims are processed. Staying informed about these changes is critical to avoid disruptions in revenue flow. Healthcare organizations must invest in training and technology to navigate these shifts seamlessly. Proactive monitoring of regulatory updates ensures adherence to guidelines, mitigates financial risks, and sustains operational efficiency in the revenue cycle process.

Patient Engagement and Satisfaction in the Revenue Cycle
Patient engagement and satisfaction are pivotal in the revenue cycle, as clear communication and transparency in billing foster trust and financial clarity, enhancing overall care experiences.
8.1 Enhancing Patient Communication for Better RCM Outcomes
Effective patient communication is crucial for improving Revenue Cycle Management (RCM) outcomes. Clear explanations of billing processes, insurance coverage, and payment options reduce misunderstandings and enhance patient trust. By providing transparent and timely updates, healthcare providers can minimize confusion and anxiety related to financial responsibilities. Additionally, offering personalized communication channels, such as patient portals or mobile notifications, empowers individuals to engage actively in their financial care journey. This proactive approach not only boosts patient satisfaction but also streamlines the revenue cycle, leading to faster and more efficient payments.
8.2 Patient-Centric Approaches to Revenue Cycle Management
Patient-centric approaches in Revenue Cycle Management (RCM) prioritize transparency, convenience, and personalized care to enhance patient satisfaction and financial outcomes. By offering tailored payment plans and clear explanations of billing processes, healthcare providers can reduce financial stress and improve patient trust. Leveraging technology, such as patient portals and mobile apps, allows patients to access billing information, make payments, and view insurance details effortlessly. These strategies not only streamline the revenue cycle but also foster long-term patient loyalty and engagement, ensuring a positive experience throughout the care journey.